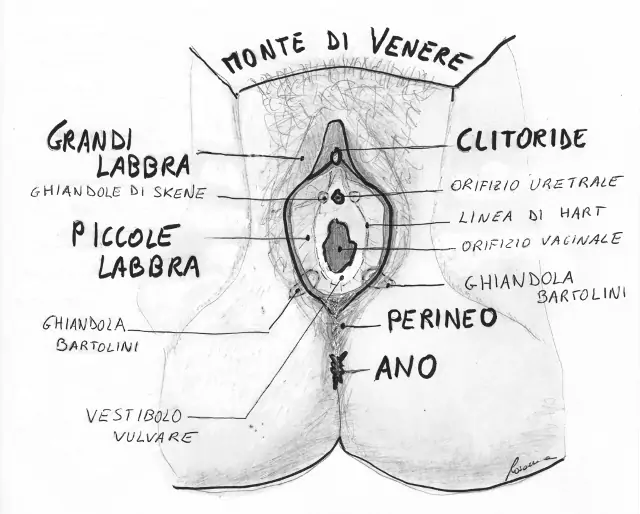
Vulvodynia is a syndrome characterized by “discomfort or vulvar burning, in the absence of visible diseases or clinically identifiable specific dysfunctions”. More often, this type of pain is described by women as “intimate burning.” If localized only to the vulvar vestibule, it is called Vestibulodynia; if the pain spreads beyond the vestibule, it is called Vulvodynia.
Vulvodynia is a very common condition that mainly affects Caucasian and African American women.
It is estimated that 12-15% of women suffer from it to varying degrees and that 14 million women have experienced this type of disorder during their lifetime.
Although Vulvodynia is quite common, it remains a little-known condition, and there are still few doctors who know how to recognize and treat it.
Search for a professional who can diagnose and treat Vulvodynia among the professionals recommended and affiliated with Cistite.info APS and discover the services offered to members.
A specific supplement can help you reduce chronic pelvic pain and the symptoms of Vulvodynia. Discover Puronerv CBG, Puronerv Oleogel and Puronerv Dol.
Symptoms
What are the symptoms of Vulvodynia?
What is the differenze between localized and generalized Vulvodynia?
Based on the symptoms, Vulvodynia can be classified into two forms:
Localized Vulvodynia (also called Vestibulodynia or "Vulvo-vestibular syndrome") where the pain is limited to the vestibular region or parts of it. It is by far the most common form of Vulvodynia, affecting 80% of women with Vulvodynia. The age of onset is predominantly during the reproductive years. It is characterized by:
- dyspareunia (pain during sexual intercourse): a stabbing sensation at the beginning of intercourse
- vulvar sensitivity (especially near the opening of the Bartholin and Skene glands, on the vestibule and the clitoris)
- fragility and variable inflammation of the vulvar tissues
- burning sensation upon pressure, feeling like contact with a hot coal
- sensation of irritation and abrasion
- sensation of small cuts on the vulva
- dryness
- sensation of pins and needles
- vulvar pulsations
- sensation of stretching / tension
- sensation that the hair around the vulva is being pulled
- vulvar edema (feeling like having a swelling or a "tube" sensation)
- the pain is predominantly provoked, meaning it occurs as a result of an external stimulus
Generalized Vulvodynia (true Vulvodynia): the pain is widespread, not limited to the vestibule, but extends throughout the vulva and sometimes beyond. It affects 20% of women with Vulvodynia and often begins in perimenopause and menopause. The most common symptoms are:
- burning sensation
- itching
- prickling sensation
- pins and needles sensation
- less frequently, pain
- dyspareunia is not as prominent as it is in Vestibulodynia
- touching the vulva causes pain that can radiate beyond the touched area, sometimes involving the urinary tract and the entire pelvic region
These symptoms are not as well-defined as in vestibulodynia; rather, they are dull, deep, and diffuse. Their onset is almost always spontaneous, meaning they are not caused by irritating stimuli, and the discomfort is continuous with brief remissions. Unlike vestibulodynia, in vulvodynia itching—often followed by typical scratching lesions—is frequently present, has a sudden and apparently unjustified onset. Visually, there are no signs of inflammation, abrasions, or ulcerations of the mucosa, which appears intact and healthy.
The boundary between one form and the other is not always so clear-cut, and the presence of one does not exclude the presence of the other.
In-depth look: Symptoms of Vulvodynia and Vestibulodynia
Causes
What are the causes of Vulvodynia?
The origin of vulvodynia is still uncertain today. However, the most widely accepted hypotheses identify three key causes in the onset of the condition: mast cell hyperactivation (especially in vestibulodynia), neurological alteration, and muscle contraction. These three etiological factors interact and influence each other, becoming both cause and consequence of one another.
- Mast cell hyperactivation
Mast cells are cells present in internal tissues (vagine, urethra, bladder, nose, mouth, lungs) that contain vesicles which, after contact with an external harmful agent, open and release their content into the tissue to defend it.
These granules contain various molecules capable of triggering inflammation, which is the normal and effective defensive response to the attack of a foreign agent, ending with its neutralization. However, if external attacks are frequent and constant (such as ongoing infections and irritations), mast cells become hypersensitive, releasing many more inflammatory substances into the tissue than necessary. This leads to a condition where inflammation and pain persist chronically, even in the absence of foreign agents.
The irritating agents that can trigger and sustain mast cell hyperactivity are numerous: infections, chemical irritants (medications, creams, excipients, additives, etc.), mechanical factors (sexual intercourse, use of internal tampons, gynecological exams, etc.), hormonal factors, estrogen-progestin contraceptives, and more.
In-depth look: Mast cell hyperactivation
- Neuropathy
In cases of neuropathic pain, the vulva appears healthy and normal, but the problem lies in the nervous system that carries sensations from the vulva. Essentially pain is present even without any apparent damage and sometimes without any triggering factor.
This pain is self-sustaining, becoming both the cause and the consequence of itself. Chronic neuropathic pain is also known as a "pain disease".
When an organism suffers for a long time, a secondary depressive condition also develops, which affects the nervous pathways, further lowering the pain threshold.
The factors potentially responsible for neuropathy are multiple and sometimes simultaneous: mast cell hyperactivation, Herpes infections, genital trauma, vulvar surgery, HPV infections and pelvic contraction.
In-depth look: Neurological alteration
- Muscle contraction
The contraction of the puboccygeus muscle develops following the release of leukotrienes by inflammatory mast cells.
This contraction compresses all the structures passing through it: urethra, vaginal introitus, anus, arteries, veins and nerves. Their compression leads to difficulties urinating, dyspareunia, constipation, reduced oxygen flow, accumulation of cellular metabolic waste in the tissues and pain (Vulvodynia, Anodynia, stranguria).
The pain itself leads to pelvic floor muscle contraction as a defense mechanism, which causes further suffering of the pelvic tissues and increasing inflammation of the pudendal nerve. This creates a vicious cycle of pain-contraction-pain-contraction.
In-depth look: Pelvic muscle contraction
Diagnosis
How is Vulvodynia diagnosed?
The diagnosis of vulvodynia is made by exclusion. It is therefore necessary to rule out all conditions that could cause the same type of pain: genital infections, abscesses of the Bartholin glands, dermatological diseases (lichen planus, lichen sclerosus, psoriasis, allergic dermatitis, contact dermatitis, etc.), vulvar tumors, neurological diseases, systemic illnesses, or hormonal changes (vaginal atrophy due to menopause or hormone therapy).
Once all these conditions are excluded, a swab test is performed: a cotton swab is used to gently touch various points on the vulva, arranged and numbered like on a clock face, to check if the light touch is perceived as painful (allodynia).
If the previously performed tests are negative, the pain has lasted for more than 3 months, and the swab test is positive, a diagnosis of vulvodynia is made:
- localized (Vestibulodynia) if the pain caused by the swab test remains confined to the touched point and/or vulvar erythema is present
- generalized if the vulvar mucosa appears normal and the pain is felt beyond the touched area
The fact that vulvodynia is a disease characterized by pain—pain that is invisible and has no clinically observable or diagnosable signs—often leads less-informed doctors to consider the problem psychosomatic, "in the patient's head." This forces women to undergo countless visits before receiving an appropriate diagnosis. Diagnostic and therapeutic delays, along with prolonged symptoms, worsen the condition, making healing more difficult and treatment longer and more complex.
A statistical survey on vulvodynia conducted by our association revealed that women with vulvodynia take on average 4 years and 8 months (!!) to receive the correct diagnosis.
In-depth look: Diagnosis of Vulvodynia
Therapy
What is the treatment of Vulvodynia?
There are various treatments for both localized and generalized vulvodynia, as the causes are diverse and multiple body areas can be involved.
In general, a doctor experienced in vulvodynia follows a treatment plan aimed at eliminating or reducing the three triggering causes:
- reduction of local inflammation to avoid further fueling the condition,
- regulation of nerve signaling to reduce pain,
- relaxation of contracted muscles (to improve the condition of the vulvar tissue, reduce friction during intercourse, prevent abrasions on the mucosa and subsequent post-coital infections and irritations, and decrease the pressure exerted by the contracted muscle on the pudendal nerve)
All of this should be accompanied by psychological treatment, which allows the patient to reclaim her sexual, social, and emotional life—areas that the condition has impacted.
Regardless of the therapy being followed, every woman affected by vulvar sensitivity must adhere to essential behavioral rules to avoid any possible irritating stimuli that could maintain or worsen the condition.
The therapeutic approach must be tailored to each individual woman. What is effective for one woman could even be harmful to another. Therefore, it may take a long time and many attempts before discovering the most effective treatments.
Although healing is often slow, it is definitely possible. However, it’s important to keep in mind that at least 6 months of treatment are usually needed before seeing significant improvements (sometimes even up to a year), and the process inevitably involves alternating periods of improvement and setbacks.
In-depth look: How to reduce local inflammation
In-depth look: How to regulate nerve signaling
In-depth look: How to relax contracted muscles
Read on the forum the Personal Stories of Vulvodynia and the Testimonials of Healing from Vulvodynia.
Bibliography
”Vulvodinia:etiopatogenesi e approccio terapeutico” Prima parte, Luciano Mariani, Filippo Murina
“Fisiopatologia, classificazione e diagnosi della dispareunia”, Graziottin A. Rovei V.
Jannini E.A. Lenzi A. Maggi M. (Eds), “Sessuologia Medica. Trattato di psicosessuologia e medicina della sessualità”, Elsevier Masson, Milano, 2007, p. 379-382
Genova Anno V - n°28 - 03.04.2007 Pagine Nazionali Aggiornamenti del 19/04/2007 “Vulvodinia”
Dott. Murina Filippo in collaborazione con: Dr. Tassan Pietro e Dr. Roberti PasqualeThe Vulvodynia Guideline, Hope et Al.2005, American Society for Colposcopy and Cervical Pathology Journal of Lower Genital Tract Disease, Volume 9, Number 1, 2005, 40–51
“Vulvodinia essenziale e vestibolite vulvare (vulvar burning syndrome), Volpicelli. 22/05/2014 http://www.fertilitycenter.it/ginecologia/vulvodinia
“Le cistiti: tutto quello che è bene sapere” Graziottin 09/03/2006 http://www.alessandragraziottin.it/it/div_scheda.php/Le-cistiti-tutto-quello-che-e-bene-sapere?ID=1174
Bjorling DE, Wang Z Yi. Estrogen and neuroinflammation. Urology, 2001; 57, 6, S1:40-46.
Aloe L, Leon A, Levi-Montalcini R. A proposed autacoid mechanism controlling mastocyte behaviour. Agents Actions, 1993; 39, S: 145-147.
UNA MEDICINA A MISURA DI DONNA CIC Edizioni Internazionali
“LA VESTIBOLITE VULVARE E IL DOLORE CRONICO” Graziottin, UNA MEDICINA A MISURA DI DONNA, CIC Edizioni Internazionali, pagg 166-173
“Vestibolite vulvare ed agopuntura: nostra esperienza” Benedetto De Pasquale, et al., Pubblicato su: Rivista di ostetricia ginecologia pratica e medicina perinatale (organo ufficiale AOGOI) Vol. XXV n° 2/3 Anno 2010 pag. 30-34, S.C. di Ostetricia e Ginecologia Azienda Ospedaliera Valtellina e Valchiavenna, Presidio Ospedaliero di Sondalo (SO) (Direttore Dott. B. De Pasquale)
“L’uso di assorbenti e le infezioni vaginali” Campagna di prevenzione Aogoi a curadi V.DubinieF.Parazzini
“SOSTANZE SENSIBILIZZANTI NEI TESSUTI”, S. Seidenari, F. Giusti Clinica Dermatologica, Università di Modena e Reggio Emilia