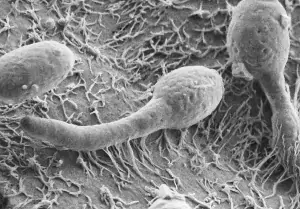
Candida is a fungus (more precisely a yeast) that is commensal, meaning it is a harmless microorganism normally present in our body at the vaginal, oral, skin, and intestinal levels, where it performs important functions such as hormonal regulation, sugar digestion, bile pigment breakdown, lowering cholesterol, and producing vitamins K, B1, and B6. In the presence of predisposing factors, candida changes form and becomes a true pathogen, taking on an elongated appearance with filaments called pseudohyphae that penetrate the deeper layers of tissues and cause a local infection.
Cistite.info has developed a specific Treatment Plan to help you fight and prevent vaginal Candida.
- Causes of Candida infection
- Symptoms of Candida
- Diagnosis of Candida
- Traditional therapy
- Natural therapy for Candida
- Miriam Protocol
Many authors classify Candida infection as a sexually transmitted disease. In reality, it should be considered an endogenous disease, meaning a condition caused by microorganisms originating from our own body and not from the outside. In fact, as long as Candida is balanced with our defenses, it remains a harmless, round, and smooth yeast. Only in the presence of predisposing factors does it change form and become pathogenic, taking on an elongated appearance with filaments called pseudohyphae that penetrate the deeper layers of tissue, causing local disease. Candida can also form spores, which are parts that detach and move away from the mother cell.
There are numerous species potentially pathogenic to humans: Candida albicans (responsible for the majority of vaginal fungal infections), glabrata, krusei, and tropicalis.
In-depth look: The Candida microorganism
Causes
What are the causes of Candida infection?
Candida, in the presence of predisposing factors, changes form and becomes pathogenic, taking on an elongated appearance with filaments that penetrate the deeper layers of tissue, causing local disease. This occurs due to various triggering factors.
- Alteration of vaginal secretion
Anything that alters vaginal secretions and the balance of the bacterial flora (hormonal contraception, menopause, pregnancy, antibiotics, excessive hygiene, increased vaginal pH) increases the likelihood of developing Candida. - Antibiotics
Antibiotic treatments also eliminate all the beneficial bacteria that protects us from Candida. Since Candida is a yeast, it is not affected by the bactericidal effect of antibiotics and will remain free to reproduce uncontrollably. - Hormonal imbalance
Candida is favored by increased progesterone (in the premenstrual phase, during pregnancy, in perimenopause, and during hormonal contraceptive therapy) and in cases of hormonal imbalance (menopause, hormone replacement therapy, surgical removal of ovaries, fallopian tubes, uterus). - Physical weakening
Other predisposing factors include all diseases or conditions that weaken the body and lower the immune system: cortisone, chemotherapy, severe chronic illnesses, AIDS, stress, sudden weight loss, anorexia, etc. - Microlesions of the genital mucosa
All conditions that damage the first layer of the genital mucosa are predisposing factors: vulvodynia, vestibulodynia, recurrent genital infections, irritations, vulvar dermatitis, vulvare dermatoses, excessive intimate hygiene, sexual intercourse without adequate lubrication, prolonged use of sanitary pads and synthetic clothing. - Intimate cleansers and douches
Intimate cleansers and vaginal douches mechanically remove the normal protective bacterial flora and cause sensitization and local irritation that further decrease the defensive capabilities of the vaginal mucosa. - Other uro-genital infections
Candida, cystitis, and vaginal infections often go hand in hand and influence each other because they progressively disrupt the local balance. - Lack of skin breathability
Synthetic clothing, sanitary pads, and panty liners do not allow the vulvar mucosa to breathe, causing maceration and moisture—ideal conditions for Candida to reproduce.
In-depth look: The triggering factors of Candida
Symptoms
What are the symptoms of vaginal Candida?
At the genital level, Candida infection causes:
- intense intimate itching (that is, vulvar and vaginal)
- intimate burning (vulvar and vaginal)
- dyspareunia (pain during sexual intercourse)
- whitish discharge resembling curdled milk
- pain during urination due to microlesions caused by scratching
- edematous (swollen) and erythematous (red) vaginal and vulvar mucosa
- vesicles and ulcers (more rare)
Candida can also affect the urethra (causing mild urethral itching, dysuria, watery discharge) or the bladder (causing typical cystitis symptoms).
In-depth look: The symptoms of Candida
Diagnosis
How is the diagnosis of vaginal Candida made?
The diagnosis of vaginal candidiasis “should” be made with a vaginal swab. Often, when faced with discharge and itching, a careless doctor simply prescribes antifungals without confirming with a vaginal swab. This leads to: development of resistance, local sensitization, therapeutic ineffectiveness, and the inability to diagnose (and treat) the real conditions responsible for the symptoms.
The diagnosis of urethral Candida is made with a urethral swab, while bladder Candida is diagnosed with a specific urine culture.
In-depth look: The diagnosis of Candida
Treatment of Candida: the failure of traditional antifungal therapy
Is traditional antifungal therapy truly effective against Candida?
Synthetic antifungal therapies (azoles and polyenes), in addition to having many side effects, some of them severe, often only manage to temporarily contain the problem, leading to continuous relapses. This happens both because its pseudohyphae reach the deeper layers of tissue, and even when the surface layer is removed, the underlying roots remain, and because fungi and yeasts tend to develop resistance to antifungals.
A good antifungal therapy should not only aim to fight Candida but also to restore local defenses, because without this recovery no antifungal treatment will ever have lasting effects, and the relapse will return more aggressively than before.
Since it is not a sexually transmitted disease and Candida is a commensal organism (we infect ourselves), treating the partner is unnecessary.
In-depth look: The failures of traditional antifungal therapy for Candida
Reconstructive treatment of Candida and natural remedies
What are the treatments and natural remedies for Candida?
Since Candida infections are always caused by a deficiency of lactobacilli, altered pH, and fragility of the mucous membranes, therapy should focus on restoring the bacterial flora, boosting immune defenses, normalizing vaginal pH, and repairing genital tissues.
In our forum over the years, we have gathered many experiences and testimonies about the most effective natural strategies to achieve all this, and we have seen that the most effective remedies are:
- Lactoferrin
- Pau d'Arco (Tabebuia avellanedae), also called lapacho
- Lactic acid bacteria
- Yogurt
- Honey
- Antioxidants
- Diet
- Modification of daily habits
- Vaginal acidifiers (Refresh gel)
- Other natural remedies such as the local application of tea tree oil, baking soda, boric acid and potassium permanganate have significant antifungal action but have proven to be very irritating to the vaginal mucosa
Cistite.info APS collaborates with specialized doctors who apply the reconstructive approach in treating Candida and vaginal infections, offering our members discounts and benefits on services. Check the list of recommended and affiliated doctors or try the free consultation service.
Miriam Protocol
What is the Miriam Protocol?
Through the experiences of the women in the Cistite.info APS forum (more than 5,000), we have developed a natural treatment plan for vaginal Candida that involves the optimized use of the natural substances described above, for a more effective and lasting reconstructive approach compared to traditional synthetic destructive therapies.
This is the “Miriam Protocol” and it consists of an oral treatment, a local treatment, and a series of behavioral recommendations.
Get the Miriam Protocol for free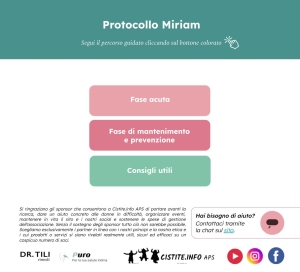
Read on the forum Personal Stories of Candida and Testimonials of Healing from Candida.
In-depth look: Candida therapy
Bibliography
- “Vaginal Candidiasis (Yeast Infection)” https://pubmed.ncbi.nlm.nih.gov/34883540/
- “Sobel JD, Faro S, Force RW, Foxman B, Ledger WJ, Nyirjesy PR, Reed BD, Summers PR. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations” https://pubmed.ncbi.nlm.nih.gov/9500475/
- “Svobodová L, Lysková P, Hamal P. Kandidovvá vulvovaginitida [Vulvovaginal candidiasis]” https://pubmed.ncbi.nlm.nih.gov/26636630/
- “Battaglia F, Mariani L, Anglana F, Milite V, Quattrini M, Plotti F, Tomao F, Plotti G. Vulvovaginiti da candida. Approccio terapeutico” https://pubmed.ncbi.nlm.nih.gov/15940073/